Diabetic Retinopathy - An Overview
Posted on: 22/May/2018 4:49:41 PM
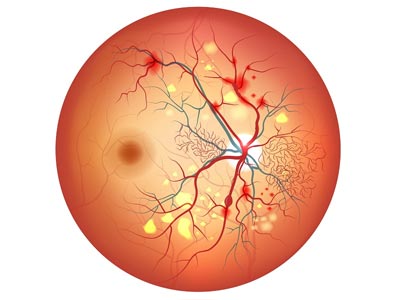
Diabetic retinopathy usually starts as a mild disease. It affects light-sensitive tissue blood vessels in the retina that lines the back of the eye. This happens among the working-age adults the common cause of vision loss in diabetics leading to vision impairment and blindness. Diabetic macular edema (DME) causes blurred vision which has no symptoms in the early stages. The disease often progresses unnoticed until it affects vision.
During the initial stages, the blood vessels in the retina become weak and small bulges are developed called microaneurysms. These may burst causing tiny blood hemorrhages on the retina. Normally they do not cause symptoms affecting the vision. Diabetics don`t develop diabetic retinopathy if the disease is less than 10 years however, it is better not to delay an eye test.
Diabetic retinopathy is caused mainly due to high blood sugar levels damaging the network of tiny blood vessels that supply blood to the retina. Abnormal retinal blood vessels bleeding causes the appearance of wavy vision and color changes �floating� spots are the other symptoms of macular edema. When blood vessels leak into the center of your eye it is Proliferative retinopathy. Blurry vision is one of the signs along with spots or floaters, or having trouble with night vision.
Usually, Vision returns to normal with glucose levels streamlined. If blurriness doesn`t go away when glucose levels are close to normal. An ophthalmologist can detect vision loss and other problems by a dilated eye exam and Visual acuity testing.
The lens of the eye swells during High blood sugar which will change the ability to see. People with diabetes may develop three major eye problems like cataracts, glaucoma, and retinopathy. Macula edema is a condition where the macula swells with fluid blurring the vision. Non-proliferative retinopathy does not require treatment, macular edema must be treated, fortunately, treatment is effective sometimes even reverses the loss of vision.
Diabetic retinopathy patients are generally asymptomatic initially, however in advanced stages the patients experience floaters, distortion or blurred vision. The earliest clinical sign of diabetic retinopathy are Micro aneurysms.
Four stages of Diabetic retinopathy:
Mild Nonproliferative Retinopathy - balloon-like swelling in small areas of the retina`s tiny blood vessels called microaneurysms occur.
Moderate Nonproliferative Retinopathy. blood vessels nourishing the retina are blocked.
Severe Nonproliferative Retinopathy. Blockage in the blood vessel increases thereby depriving parts of the retina with blood supply which further signals the body`s need for nourishment by growth of new blood vessels.
Proliferative Retinopathy. The new abnormal and fragile blood vessels grow along the retina that fills the inside of the eye. they do not cause symptoms or vision loss. However, blood vessels have thin, fragile walls which could leak blood leading to vision loss and even blindness.
There is no cure for diabetic retinopathy. Laser treatment (photocoagulation) is used largely for preventing vision loss before the retina gets severely damaged. Surgically removing g the vitreous gel (vitrectomy) also helps vision improvement, provided the retina is not severely damaged.
It is possible to live a normal life with diabetesif sufferers eat healthily and take exercise and manage medication (if needed) well. ... Left untreated, diabetes can cause blindness, heart disease, stroke, nerve damage (sometimes leading to ulcers and even amputation of limbs), and kidney failure.
Diagnosis
In the early stages, diabetic retinopathy does not cause any noticeable symptoms. Therefore, it tends to be diagnosed as a result of a diabetic eye screening test. This would include a comprehensive eye exam including a slit lamp examination, a dilated retinal check,and measure of your intraocular pressure. Thereafter additional tests like a Fundus Fluorescein Angiography (FFA), Ultrasound B-Scan or an Optical Coherence Tomography to study the structure of the eye may be done.
Treatment
Laser Treatment: Lasers are widely used in treating diabetic retinopathy and is performed as an out-patient procedure. In this treatment, an intense beam of light is focused on the area to be treated with the aid of the slit lamp and a special contact lens. This will reduce the retinal thickening and stops bleeding. Additional treatment may be required depending on the patient�s condition.
Surgical Treatment: In some patients, the vitreous may pull on the retina reducing vision severely. In such cases, a surgical procedure called vitrectomy is performed. This surgery is done for advanced stage of Diabetic Retinopathy.
Intravitreal injections: This may be recommended in selected conditions. The drug injected would depend on your condition and your doctor would discuss the same with you.